Menu

Group Leader: Fabio Grassi
Researchers: Elisa Civanelli, Benedetta De Ponte Conti, Tanja Rezzonico Jost, Lisa Perruzza, Matteo Raneri, Morena Scantamburlo
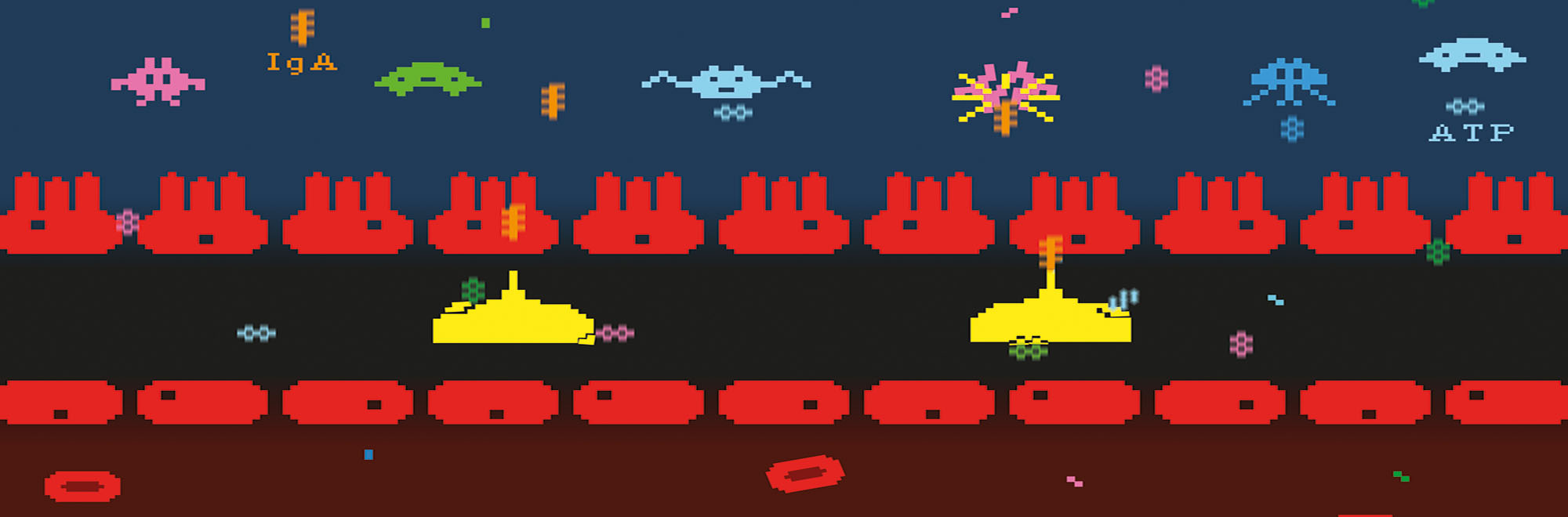
The human gastrointestinal (GI) tract is a complex ecological niche, in which all the three domains of life (Archaea, Bacteria and Eukarya) and Viruses co-exist in close association with the host. This complex microbial community, referred to as the gut microbiota, has co-evolved with the host in a mutualistic relationship that influences many physiological functions such as energy harvesting, development and function of the immune system. The subtle equilibrium between the gut microbiota and the host is a key element in human health.
In fact, alterations in the composition of the microbial community structure, termed dysbiosis, have been associated to an increasing number of medical conditions. Since the immune system and the gut microbiota start developing together at birth, it has been hypothesized that their co-evolution selects and maintains mutualistic or symbiotic microorganisms within the GI niche. Central in this homeostatic relationship is the local production of immunoglobulin A (IgA), which is the most copious Ig isotype produced by the human immune system.
IgA interaction with the polymeric Ig receptor (pIgR) and luminal secretion guarantee mucosal protection by entrapping microorganism in the mucus, neutralizing invading pathogens and microbial inflammatory compounds. Adenosine triphosphate (ATP) is a ubiquitous extracellular messenger, which activates purinergic receptors in the plasma membrane termed P2 receptors. The P2X7 receptor subtype is an ATP-gated nonselective cationic channel expressed in a variety of cell types. In T cells protracted receptor stimulation leads to cell death. P2X7 plays a crucial role in regulating Tfh cells abundance and thereby T dependent secretory IgA (SIgA) and microbiota composition. We investigate different aspects of the extracellular ATP (eATP)/P2X7 axis in regulating host/microbiota mutualism in the gut.
Projects
Group leader: Fabio Grassi
Researchers: Tanja Rezzonico Jost, Research assistant
Status: In progress
The aim of this project is to develop an implantable biochip system to investigate the complexity of drugs/biomarkers relationships in chronic inflammatory diseases. To reach this goal, a multidisciplinary approach is needed because the system requires: (i) The development of an innovative sensor to detect an array of drugs, including nanotechnology and system level integration to improve sensor specificity; (ii) The development of new micro-electronics technology to decrease chip size for implantation in mice as well as a convenient chip remote powering data transmission; (iii) Testing in murine models of chronic inflammation; (iv) Investigating the pharmacokinetics of biochemical enzymes-substrates to identify the best cytochrome P450 isoforms, out of more than 3,000 possibilities, to be integrated onto the biochip in order to ensure the detection of those exogenous and endogenous compounds which are relevant for the specified medical application. To best address all of these multidisciplinary demands, the project partnership includes experts in: (i) Nano-sensing, with a special focus on P450 biosensors (S.Carrara/EPFL), (ii) Chip fabrication with focus on implantable systems (Dehollain /EPFL), (iii) Biomarker variations (our group), (iv) Pharmacokinetics (Von Mandach/University of Zurich Hospital).
Group leader: Fabio Grassi
Status: In progress
Class switch recombination (CSR) is an irreversible somatic recombination mechanism by which B cells switch their surface immunoglobulin class expression from IgM and IgD to other isotype with distinct effector function. This diversification is essential for a protective adaptive humoral immune response. B cell receptor (BCR) activation together with exogenous signals, including tumor necrosis factor (TNF) family members, Toll-like receptors (TLRs) ligands or cytokines trigger CSR. We have shown that extracellular adenosine critically contributes to CSR in murine mature B cells. Murine naïve B cells release ATP upon coordinate B cell receptor (BCR) and Toll Like Receptors (TLRs) stimulation. The released ATP is hydrolysed to adenosine by plasma membrane ectonucleoside triphosphate diphosphohydrolase 1 (ENTPD1) CD39 and ecto-5′-nucleotidase (5’-NT) CD73. Remarkably germinal center and isotype switched B cells display higher expression of CD73. Moreover, CD39 and CD73 deficient B cells showed in vitro a significant impairment in their capacity to differentiate to class switch plasma cells upon BCR and TLR engagement, underlying the role of adenosine in the B cells isotype switching process. Ig CSR-deficiencies in human can be dependent from an intrinsic B cell defect, however most of them are still molecularly undefined and diagnosed as common variable immunodeficiency (CVID). Notably, CVID patients with impaired class switched antibody responses are selectively deficient in CD73 expression in B cells, suggesting that CD73 dependent adenosine generation contributes to the pathogenesis of this disease.

Via Vincenzo Vela 6
6500 Bellinzona, Switzerland
Tel. +41 91 820 0300
Fax +41 91 820 0302
Facebook / Twitter
